SLAC, Stanford Team Focuses on High-Energy Electrons to Treat Cancer
Accelerator physicists at SLAC and cancer specialists from Stanford are working on a new technology that could dramatically reduce the time needed for cancer radiation treatments.
By Diane Rezendes Khirallah
Accelerator physicists at SLAC and cancer specialists from Stanford are working on a new technology that could dramatically reduce the time needed for cancer radiation treatments. The team ran an initial experiment using high-energy electrons in January and has asked the National Institutes of Health for $1.25 million to finance further studies.
As Eric Colby, SLAC’s director of accelerator research, put it, “While the result is extremely preliminary – people won't be lining up for treatment anytime soon – it is a great example of the sort of innovative, high-social-value research that SLAC and Stanford are capable of, and is the start of what we hope will be a growing collaboration.”
It all started when Dr. Billy W. Loo, a radiation oncologist at Stanford University School of Medicine, read a paper in Physics and Medicine in Biology that proposed using high-energy electrons, rather than X-rays, for radiation therapy. Loo realized that with the right delivery system, this could reduce the typical length of a radiation treatment from the current average of 15 to 60 minutes down to less than a second for a wide range of tumors.
He discussed the idea with his close collaborator, medical physicist Peter Maxim, and then asked Magdalena Bazalova, a radiation oncology instructor on his staff, to run computer simulations to see if the method could work.
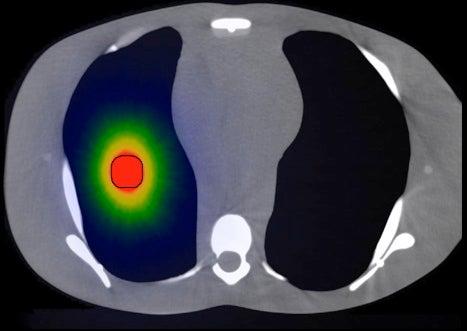
Bazalova had become an expert in a technique called Monte Carlo simulation while working in high-energy physics at CERN, the European center for particle physics. Named after the gambling mecca in Monaco, Monte Carlo simulations use multiple, repeated random data points as square one for predicting outcomes. In her initial report to Loo, Bazalova said the simulations confirmed that high-energy electrons should provide more targeted treatment than photons of X-ray light.
His email response came back in less than 10 minutes: “Holy smokes! We definitely need to talk more about this.”
Loo and Maxim knew SLAC had a beam line – the Next Linear Collider Test Accelerator, NLCTA – staffed by researchers with experience in supporting small accelerator physics experiments. What’s more, when they approached SLAC, they learned that Sami Tantawi, associate professor of particle physics and astrophysics at the lab, had independently come up with the idea of building a machine to treat cancer with high-energy electrons. His ultimate goal was to shrink it to table-top size, small enough for use in a patient-care suite.
The Stanford and SLAC groups quickly teamed up and decided to apply for an NIH grant to finance a research program. The application deadline loomed just days away, and they would first need to demonstrate that they were capable of carrying out experiments. Would that allow enough time to design an experiment, reconfigure the NLCTA accelerator, source the necessary materials, run the experiment and analyze the initial data?
And of course, there’s the matter of getting time on the NLCTA beam, which can be very competitive.
“We were asked to help with an urgent experiment. When the boss asks a question like that, the answer is ‘yes,’” said SLAC engineering physicist Keith Jobe, who would pull the team together and manage the logistics. “And furthermore, it’s exciting.”
The team would need to simulate a patient-treatment suite for radiation therapy. Jobe and his colleagues from the Test Facilities Department removed a section of the beam line at NLCTA and installed special windows.
They ran the experiment using “phantoms” that mimic human tissue – in this case, specially designed layers of polystyrene with sheets of radiation-sensitive film between them.
They hit the plastic layers with the high-energy electron beam, producing dark areas on the film. The results – the locations, sizes and darkness of the exposed spots – were consistent with what the simulation predicted, offering a proof of concept that high-energy electrons could one day be successful in targeting cancer cells.
It was a collaboration of parallel interests, said Jobe, and the team moved quickly: From the date of Loo’s initial request to reviewing the data, less than two weeks elapsed.
“Everything clicked in very fast. All the right people appeared at the right moment. Everything fell into place,” Tantawi said. “The investment (the country is making) in high-energy physics is paying off in other fields that are unexpected.”
What’s next? Bazalova says there will be more Monte Carlo simulations, more testing using phantoms, and later, in vitro testing with various cell lines.
Within the radiation physics community, there is a great desire to conduct similar experiments, Jobe said. “It was a spectacular team effort.”
(Image courtesy Stanford School of Medicine, Department of Radiation Oncology)